Afib Reading of of 0.786 and Rmssd of 0.205
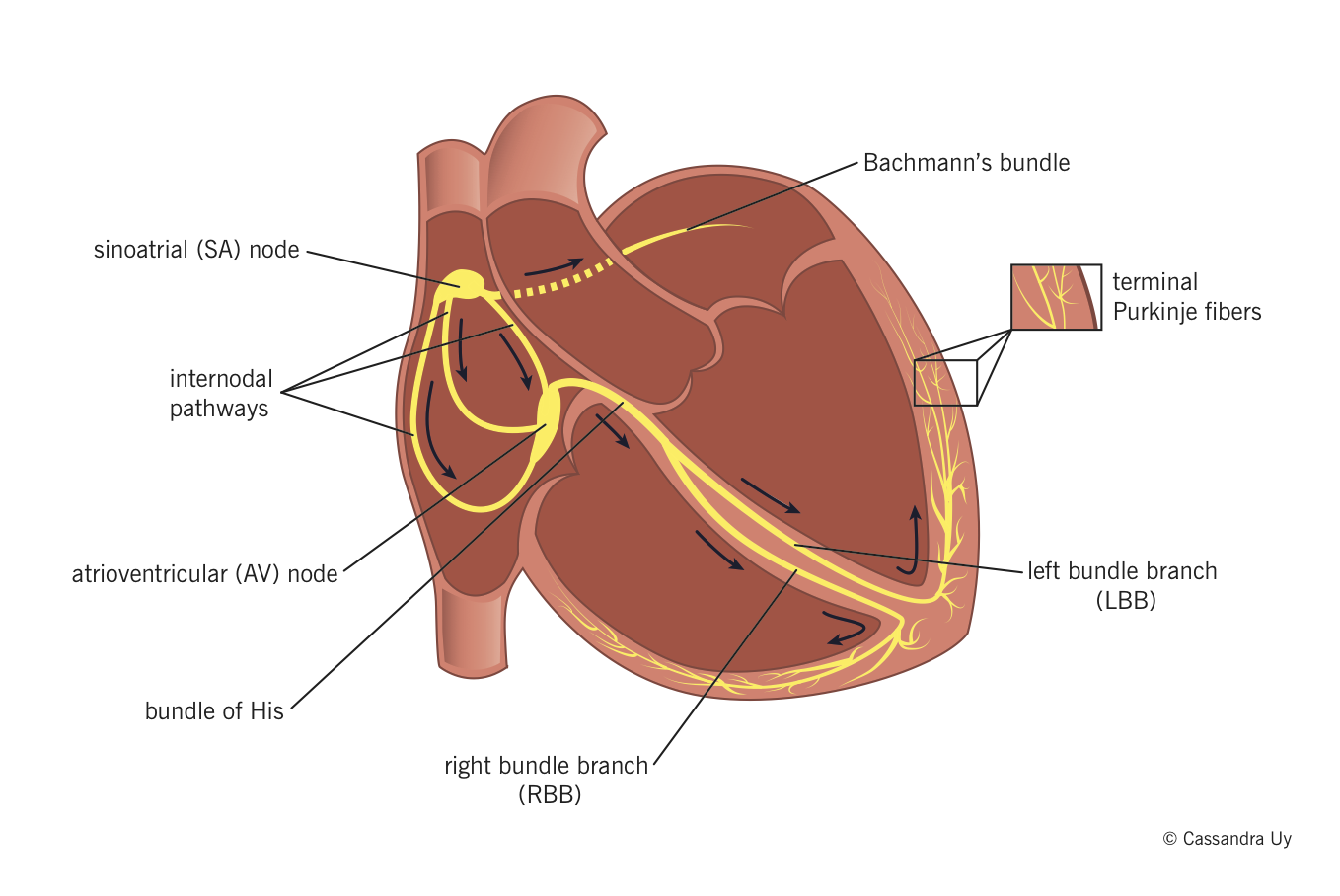
Cardiac conducting system
Clin Anat. 2009 January;22(ane):99-113.
Can J Anaesth. 1993 Nov;xl(11):1053-64.
- Sinoatrial (SA) node usually generates the action potential, i.e. the electrical impulse that initiates contraction.
- The SA node excites the correct atrium (RA), travels through Bachmann'southward bundle to excite left atrium (LA).
- The impulse travels through internodal pathways in RA to the atrioventricular (AV) node.
- From the AV node, the impulse then travels through the bundle of His and down the package branches, fibers specialized for rapid transmission of electrical impulses, on either side of the interventricular septum.
- Right package co-operative (RBB) depolarizes the right ventricle (RV).
- Left parcel branch (LBB) depolarizes the left ventricle (LV) and interventricular septum.
- Both package branches terminate in Purkinje fibers, millions of small fibers projecting throughout the myocardium.
An organized rhythmic contraction of the eye requires acceptable propagation of electric impulses along the conduction pathway. Of note, the impulses in the His-Purkinje system travel in such a way that papillary muscle contraction precedes that of the ventricles, thereby preventing regurgitation of claret period through the AV valves.
Electrophysiology
Physiol Rev. 2005 Oct;85(4):1205-53.
Ion channels
Center Rhythm. 2010 Jan;7(1):117-26.
- Ii main forces drive ions across prison cell membranes:
- Chemic potential: an ion will movement down its concentration slope.
- Electric potential: an ion will motility away from ions/molecules of similar charge.
- The transmembrane potential (TMP) is the electric potential difference (voltage) between the inside and the outside of a cell. When in that location is a net motion of +ve ions into a jail cell, the TMP becomes more than +ve, and when at that place is a net motion of +ve ions out of a jail cell, TMP becomes more –ve.
- Ion channels aid maintain ionic concentration gradients and charge differentials betwixt the inside and outside of the cardiomyocytes.
Backdrop of cardiac ion channels
- Selectivity : they are merely permeable to a single type of ion based on their physical configuration.
- Voltage-sensitive gating: a specific TMP range is required for a particular channel to be in open configuration; at all TMPs outside this range, the aqueduct volition be closed and impermeable to ions. Therefore, specific channels open and close as the TMP changes during jail cell depolarization and repolarization, assuasive the passage of different ions at dissimilar times.
- Fourth dimension-dependence: some ion channels (importantly, fast Na+ channels) are configured to close a fraction of a second after opening; they cannot be opened again until the TMP is back to resting levels, thereby preventing further excessive influx.
Annotation: The dissimilar types of cardiac ion channels are discussed below, throughout the description of the phases of action potentials in different cardiac cells.
Action potentials and impulse conduction
Physiol Rev. 2005 Oct;85(4):1205-53.
Action potential: electrical stimulation created past a sequence of ion fluxes through specialized channels in the membrane (sarcolemma) of cardiomyocytes that leads to cardiac wrinkle.
Activeness potential in cardiomyocytes
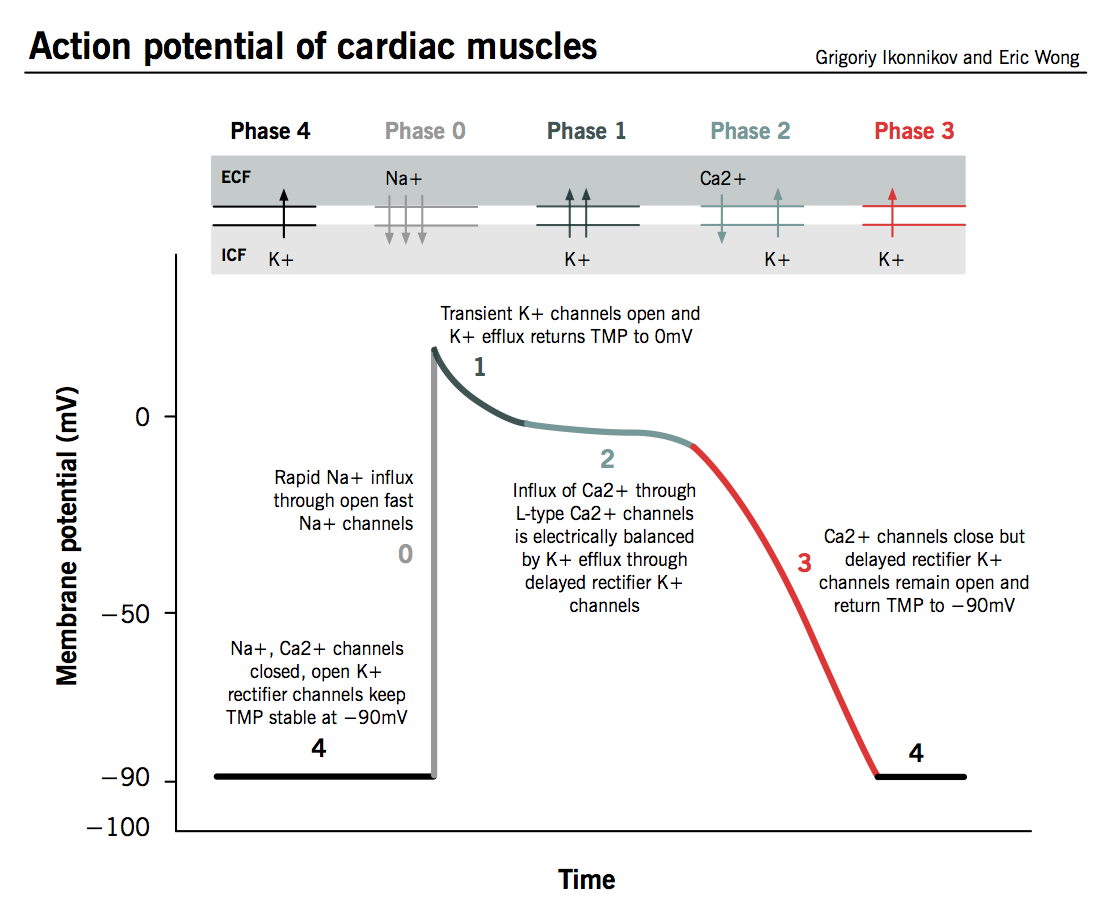
The action potential in typical cardiomyocytes is composed of v phases (0-four), commencement and ending with phase 4.
Phase four: The resting phase
- The resting potential in a cardiomyocyte is −xc mV due to a constant outward leak of Chiliad+ through inward rectifier channels.
- Na+ and Ca2+ channels are airtight at resting TMP.
Stage 0: Depolarization
- An activity potential triggered in a neighbouring cardiomyocyte or pacemaker cell causes the TMP to rise to a higher place −90 mV.
- Fast Na+ channels showtime to open one by one and Na+ leaks into the cell, further raising the TMP.
- TMP approaches −70mV, the threshold potential in cardiomyocytes, i.east. the point at which enough fast Na+ channels accept opened to generate a self-sustaining inward Na+ electric current.
- The large Na+ electric current apace depolarizes the TMP to 0 mV and slightly above 0 mV for a transient menstruation of time called the overshoot; fast Na+ channels close (call up that fast Na+ channels are fourth dimension-dependent).
- 50-type ("long-opening") Ca2+ channels open up when the TMP is greater than −40 mV and cause a pocket-sized but steady influx of Ca2+ down its concentration gradient.
Phase ane: Early repolarization
- TMP is now slightly positive.
- Some Yard+ channels open up briefly and an outward period of K+ returns the TMP to approximately 0 mV.
Stage 2: The plateau stage
- L-blazon Caii+ channels are still open and there is a small-scale, constant inward current of Caii+. This becomes significant in the excitation-wrinkle coupling process described below.
- Chiliad+ leaks out down its concentration gradient through delayed rectifier One thousand+ channels.
- These ii countercurrents are electrically balanced, and the TMP is maintained at a plateau but below 0 mV throughout phase 2.
Phase three: Repolarization
- Ca2+ channels are gradually inactivated.
- Persistent outflow of Thou+, at present exceeding Ca2+ inflow, brings TMP back towards resting potential of −90 mV to set the cell for a new cycle of depolarization.
- Normal transmembrane ionic concentration gradients are restored by returning Na+ and Ca2+ ions to the extracellular environment, and K+ ions to the cell interior. The pumps involved include the sarcolemmal Na+-Ca2+ exchanger, Catwo+-ATPase and Na+-K+-ATPase.
Action potential in cardiac pacemaker cells
Pharmacol Ther. 2005 Jul;107(1):59-79.
Drugs. 2007;67 Suppl two:15-24. (The funny current)
- Automaticity: unlike other cardiomyocytes, pacemaker cells do not crave external stimulation to initiate their action potential; they are capable of cocky-initiated depolarization in a rhythmic fashion. This property is known equally automaticity, whereby the cells undergo spontaneous depolarization and an action potential is triggered when threshold voltage is reached.
- Unstable membrane potential: Pacemaker cells have an unstable membrane potential and their activity potential is not ordinarily divided into divers phases.
- No rapid depolarization phase: Pacemaker cells have fewer inward rectifier K+ channels than exercise other cardiomyocytes, and then their TMP is never lower than −60 mV. As fast Na+ channels demand a TMP of −90 mV to reconfigure into an active state, they are permanently inactivated in pacemaker cells so there is no rapid depolarization stage.
Tabular array one. Cardiac cell types displaying pacemaker beliefs.
| Pacemaker | Location | Inherent rate (beats per infinitesimal, BPM) |
| Sinoatrial (SA) node | Right atrium (RA) at junction with superior vena cava (SVC) | 60-100 BPM |
| Atrioventricular (AV) node | RA at posteroinferior area of interatrial septum | 40-lx BPM |
| Purkinje fibers and ventricular cardiomyocytes | Throughout the ventricles | 20-xl BPM |
The sequence of events for pacemaker action potential:
- Spontaneous flow of ions mainly through deadening Na+ channels slowly depolarizes TMP in a higher place −sixty mV. This is chosen the funny current (also known every bit pacemaker current); it is active at TMPs of less than −55 mV.
- At TMP −55 mV, T-type Caii+ channels open up and go along slow depolarization.
- TMP −40 mV is the threshold potential for pacemaker cells. L-type Ca2+ channels open up and depolarize cell to 0 mV, then overshoot to +40 mV.
- Delayed rectifier K+ channels counteract the L-type Ca2+ channels for a brief plateau phase and and so return the TMP back to −60 mV as Ca2+ channels shut.
Implications of pacemaker activity on global cardiac depolarization
- Synchronous contraction: all cardiomyocytes (including pacemaker cells) are electrically coupled through gap junctions. An action potential in 1 cell will cause all neighbouring cells to depolarize, allowing the eye chambers to act equally a unit of measurement.
- Dominance: the cell with the highest inherent charge per unit of pacemaker action will therefore also set the heart rate, as all other pacemaker cells will be depolarized and rendered inactive past this stimulus.
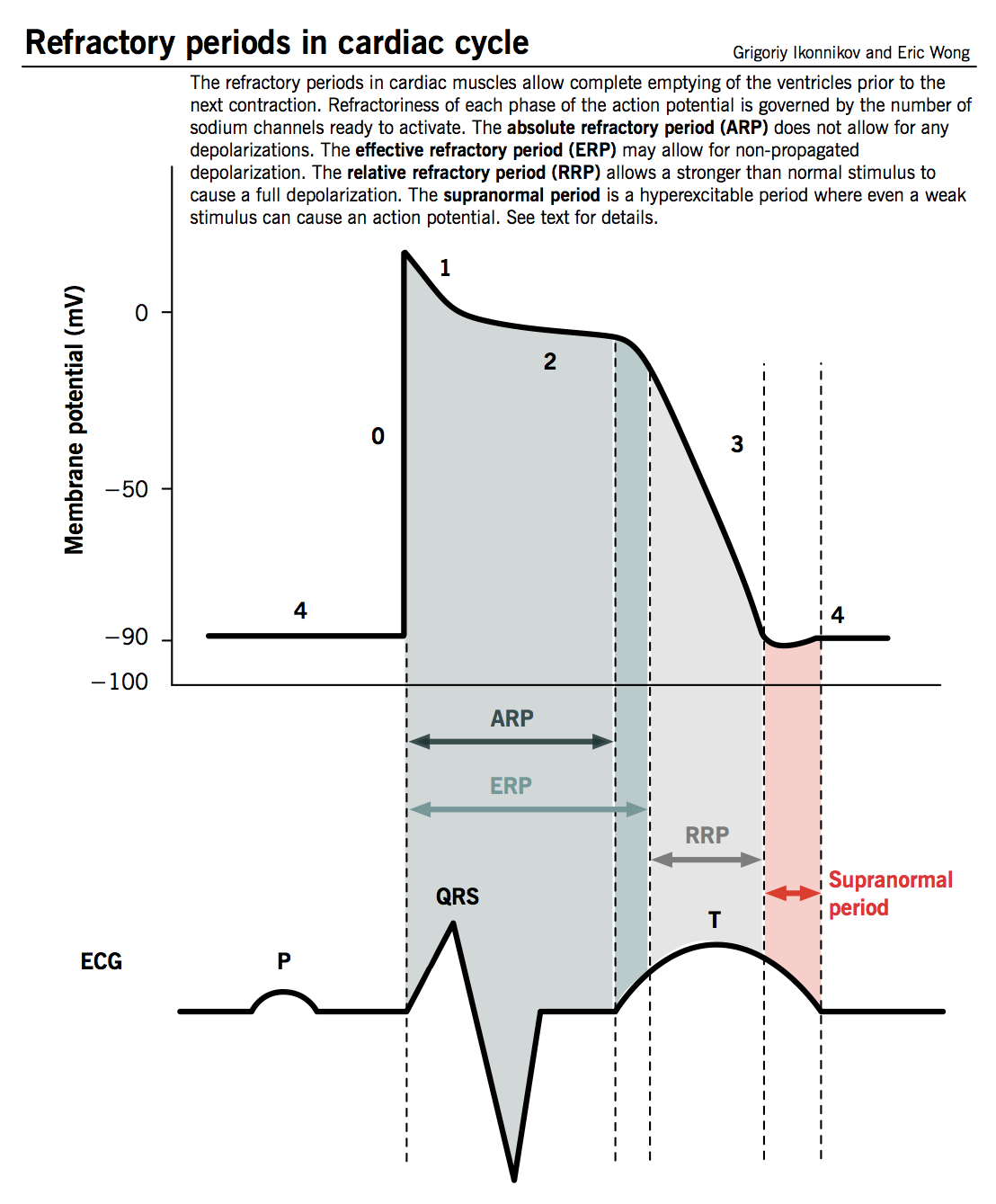
Refractory menses
- Defined as the time from phase 0 until the next possible depolarization of a myocyte, i.east. one time plenty fast Na+ channels have recovered (as TMP decreases below −fifty mV).
- Cardiomyocytes have a longer refractory menstruation than other muscle cells given the long plateau from tiresome Ca2+ channels (phase 2). This is a physiological mechanism allowing sufficient time for the ventricles to empty and refill prior to the next contraction.
- Unlike degrees of refractoriness are encountered during an activeness potential, reflecting the number of fast Na+ channels that have recovered from their inactive country and are capable of reopening.
- Absolute refractory period (ARP) : the prison cell is completely unexcitable to a new stimulus.
- Effective refractory period (ERP): ARP + short segment of phase three during which a stimulus may cause the cell to depolarize minimally but volition not result in a propagated action potential (i.eastward. neighbouring cells volition not depolarize).
- Relative refractory period (RRP): a greater than normal stimulus will depolarize the cell and cause an activity potential.
- Supranormal period: a hyperexcitable period during which a weaker than normal stimulus will depolarize the cells and crusade an action potential. Cells in this phase are particularly susceptible to arrhythmias when exposed to an inappropriately timed stimulus, which is why one must synchronize the electrical stimulus during cardioversion to forbid inducing ventricular fibrillation.
Sequence of depolarization
- The SA node unremarkably initiates electrical activation.
- The impulse propagates through atrial tissue to the AV node. At that place is no direct electrical connection between the atrial and ventricular chambers other than through the AV node, as fibrous tissue surrounds the tricuspid and mitral valves. AV node allows a very short delay in conduction (approximately 0.1 second) because it is composed of slower conducting fibers. This intermission has 2 important purposes:
- Allows the atria fourth dimension to contract and fully empty prior to ventricular stimulation.
- Allows the AV node to human action every bit a gatekeeper, limiting the transmission of ventricular stimulation during abnormally rapid atrial rhythms.
- Later crossing the AV node, the impulse spreads into the rapidly conducting bundle of His and through the bundle branches to the Purkinje fibers. The electrical impulse is distributed throughout the bulk of the ventricular myocyte for precisely timed stimulation and contraction of the ventricles.
Excitation-contraction coupling
Nature. 2002 January 10;415(6868):198-205.
Excitation-contraction coupling represents the procedure past which an electrical action potential leads to contraction of cardiac muscle cells. This is accomplished by converting a chemic indicate into mechanical energy via the action of contractile proteins.
Calcium is the crucial mediator that couples electric excitation to physical contraction by cycling in and out of the myocyte's cytosol during each activeness potential.
Contractile proteins
Main contractile elements:
- Myosin: thick filaments with globular heads evenly spaced along their length; contains myosin ATPase.
- Actin: smaller molecule (thin filaments) consisting of two strands arranged every bit an blastoff-helix, woven betwixt myosin filaments.
Regulatory elements:
- Tropomyosin: double helix that lies in the groove between actin filaments. Information technology prevents contraction in the resting state by inhibiting the interaction between myosin heads and actin.
- Troponin: complex with iii subunits that sits at regular intervals along the actin strands.
- Troponin T (TnT) – t ies troponin complex to actin and tropomyosin molecules.
- Troponin I (TnI) – i nhibits action of ATPase in actin-myosin interaction.
- Troponin C (TnC) – binds c alcium ions that regulate contractile process.
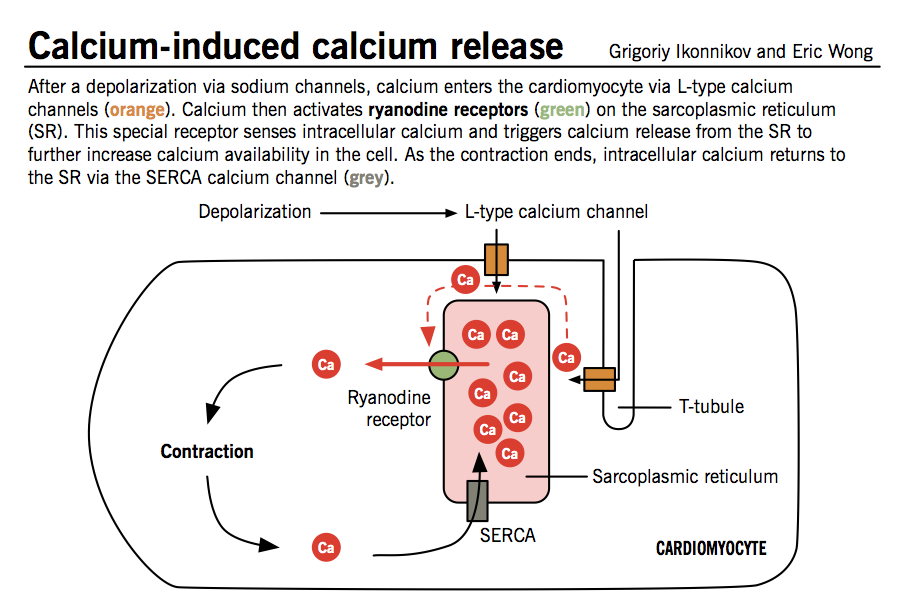
Calcium-induced calcium release (CICR)
The initial influx of Ca2+ into myocytes through L-type Ca2+ channels during phase two of the action potential is insufficient to trigger contraction of myofibrils. This indicate is amplified past the CICR mechanism, which triggers much greater release of Ca2+ from the sarcoplasmic reticulum.
- The prison cell membrane of cardiomyocytes, called sarcolemma, contains invaginations (T-tubules) that bring Fifty-type Ca2+ channels into close contact with ryanodine receptors, specialized Ca2+ release receptors in the sarcoplasmic reticulum (SR).
- When Ca2+ enters the cells through Fifty-type channels, ryanodine receptors change conformation and induce a larger release of Catwo+ from abundant SR stores.
- Large levels of intracellular Catwo+ human activity on tropomyosin complexes to induce myocyte contraction.
Contractile cycle
- Ca2+ binds to TnC → TnI is inhibited → conformational modify in tropomyosin that exposes active site between actin and myosin.
- Myosin heads collaborate with active sites on actin filaments and "flex," like oars on a boat, to "row" myosin along actin in an ATP-dependent reaction:
- Hydrolysis of ATP by ATPase on myosin (no longer inhibited by TnI) induces crossbridge formation between myosin head and agile site on actin. The strength of cardiac contraction is proportional to the number of crossbridges formed.
- Interaction betwixt myosin head and actin trigger "firing" of myosin head, causing it to pull itself along the actin filament in a process known as the power stroke.
- ADP is released from the myosin caput, which then binds a new ATP, releasing the actin filament.
- The cycle can and then repeat itself, allowing myosin to travel further along the actin molecules and progressively shorten the muscle fibers, as long every bit (i) the cytosolic Catwo+ concentration remains sufficiently loftier to inhibit the action of TnI and (ii) there is enough ATP to drive crossbridge formation.
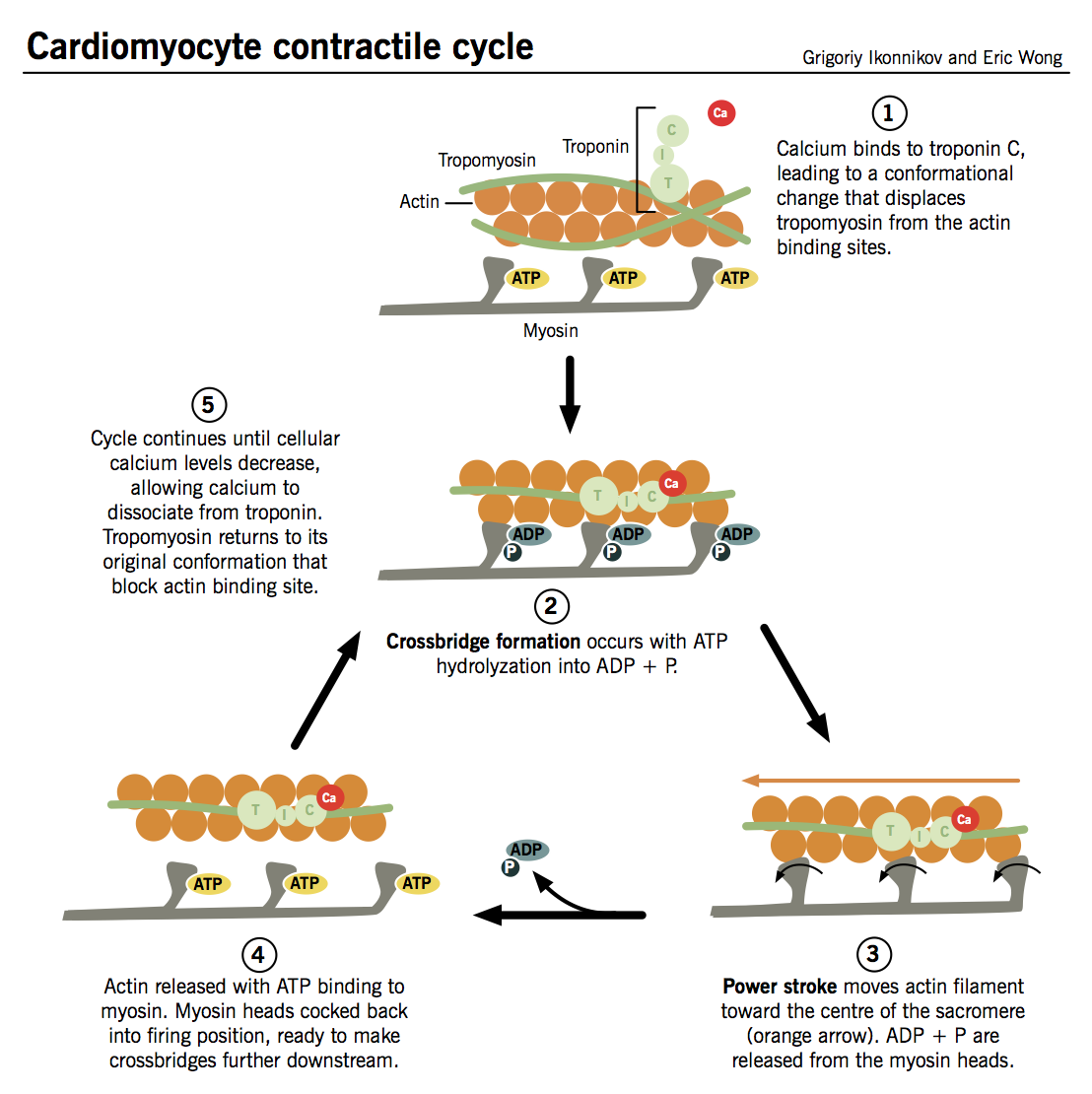
Myocyte relaxation
As with myocyte contraction, this process is synchronized with the electrical activity of the cell.
- L-blazon Ca2+ channels inactivate toward the end of phase 2 → Caii+ influx arrests → CICR trigger is abolished.
- At the same time, Catwo+ is sequestered back into the SR by sarcoplasmic reticulum Ca2+ ATPase (SERCA) and pumped out of the cell to a lesser extent by specialized Ca2+ pumps.
- Ca2+ ions dissociate from TnC as their intracellular concentration falls, and tropomyosin inhibition of actin-myosin interaction is restored.
Neural modulation of contractility
Adv Physiol Educ. 2011 Mar;35(1):28-32.
- Heart is innervated past both parasympathetic and sympathetic afferent and efferent neurons.
- Sympathetic: postganglionic sympathetic fibers from paravertebral sympathetic ganglia associated with T1-T5 innervate the atria, ventricles, and conduction organisation.
- Parasympathetic: parasympathetic innervation is limited to vagal efferent fibers which innervate the SA node and the AV node; parasympathetic innervation to the ventricles is minimal.
- Both sympathetic and parasympathetic tone is exerted on the center at rest, just parasympathetic tone predominates.
- Sympathetic neurons release norepinephrine, a catecholamine, which activates β1 receptors on cardiac myocytes, leading to the post-obit effects (note: epinephrine, also a catecholamine, can be made past the adrenal glands and released into the apportionment, and has the aforementioned upshot on β1 receptors):
- Chronotropic: increased heart rate
- Dromotropic: faster conduction through AV node
- Inotropic: increased contractility
- Lusitropic: faster relaxation after contraction
- Parasympathetic neurons release acetylcholine, a cholinergic hormone, which activates muscarinic M2-receptors on cardiac myocytes, leading to but one primary upshot:
- Negative chronotropic: decreased centre rate
Source: http://www.pathophys.org/physiology-of-cardiac-conduction-and-contractility/
0 Response to "Afib Reading of of 0.786 and Rmssd of 0.205"
Post a Comment